Understanding Thyroid Disease and Thyroid Medication

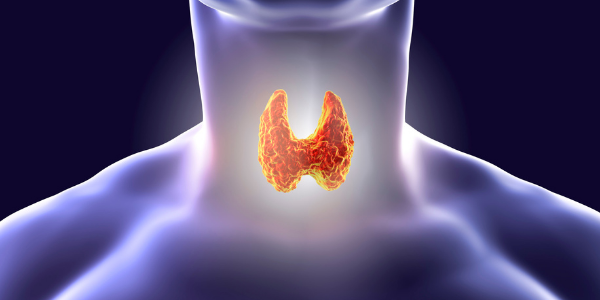
The thyroid is a butterfly-shaped gland at the base of the neck. It produces two main hormones:
- Triiodothyronine (T3)
- Thyroxine (T4)
These hormones play a crucial role in maintaining body composition, regulating metabolism, aiding growth and development, and more.
Thyroid disease affects the way the thyroid produces hormones.
- Hypothyroidism occurs when the thyroid is underactive and produces too little thyroid hormone.
- Hyperthyroidism occurs when the thyroid is overactive and produces too much thyroid hormone.
Read on to learn more about thyroid disease and the medications used to treat hyperthyroidism and hypothyroidism.
How to Know if You Have Thyroid Disease
Because thyroid hormones are so important to the body, there are clear symptoms of thyroid disease. If your thyroid isn’t functioning properly, you may experience some or all of these symptoms.
Hypothyroidism symptoms include:
- Weight gain and changes in body composition
- Sluggishness and lack of energy
- Dry skin
- Brittle hair and nails
- Fatigue and lethargy
- Sensitivity to cold
- Gastrointestinal issues like constipation
Hyperthyroidism symptoms include:
- Weight loss
- Nervousness, anxiety, and shakiness
- Rapid heartbeat and heart palpitations
- Insomnia
- Mood swings and difficulty regulating mood
- Muscle weakness and general tiredness
- Sensitivity to heat
- Gastrointestinal issues like diarrhea
Recognizing symptoms is a start.
For an official diagnosis, you typically need comprehensive lab work focusing on thyroid health and a consultation with a medical provider.
Recommended blood tests include:
This test measures the amount of free T3 in the blood.
Reverse T3 is a byproduct of thyroid hormone metabolism, and it gives your provider an understanding of how your body utilizes thyroid hormones.
This test measures the amount of free T4 in the blood.
High levels of these antibodies point to thyroid disease.
Thyroglobulin is a protein found within the thyroid, and its antibodies can indicate a thyroid condition.
Common Thyroid Diseases
We’ve discussed how you can have underactive thyroid (hyperthyroidism), or overactive thyroid (hyperthyroidism). But there are many thyroid diseases depending on the cause of the condition.
Hashimoto’s Disease
This disease occurs when the immune system begins attacking the thyroid. This can cause inflammation and the death of thyroid cells. The thyroid becomes underactive, and patients experience hypothyroidism symptoms.
Hashimoto’s Disease is most common in middle-aged women, and treatment is typically Thyroid Hormone Replacement Therapy. Patients who begin supplementing with thyroid hormones almost always report improvement of symptoms.
Idiopathic Myxedema
Idiopathic myxedema is advanced, unaddressed hypothyroidism. It also refers to the swelling (myxedema) that can occur when this condition is left untreated.
Idiopathic Myxedema is typically treated by Thyroid Hormone Replacement Therapy. Depending on the severity of symptoms, steroid treatment may also be prescribed to ease inflammation and swelling.
For serious cases, hospitalization and breathing support may be required.

Thyroiditis
Thyroiditis is swelling and inflammation of the thyroid gland. It typically causes the thyroid to leak hormones, and then impairs the thyroid’s ability to secrete T3 and T4.
Thyroiditis is caused by many things. It can be triggered by an immune condition like Hashimoto’s Disease. It can also be caused by infection and disease, as well as certain medications like Interferon (a treatment for cancer and viral infections) and Amiodarone (a treatment for serious heart arrhythmia).
Swelling and inflammation caused by thyroiditis can be treated with steroids. If triggered by a virus or infection, treating the root cause should help ease thyroiditis symptoms.
If thyroiditis is caused by an ongoing condition like Hashimoto’s Disease, Thyroid Hormone Replacement Therapy may be necessary.
Graves’ Disease
This condition is an autoimmune disorder that leads to hyperthyroidism. Similar to Hashimoto’s Disease, it occurs when the immune system attacks healthy thyroid cells.
Unlike Hashimoto’s Disease, Graves’ Disease causes an overproduction of thyroid hormone.
Graves’ Disease may also cause an eye condition called Graves’ ophthalmopathy. This occurs when the immune system begins attacking eye cells as well as thyroid cells. It may lead to bulging, swollen eyes, sensitivity to light, and a feeling of pain or pressure in the eye sockets.
Graves’ Disease is typically treated by medications like Carbimazole and Propylthiouracil, which slow the thyroid’s production of hormones. Radioactive Iodine is another treatment that destroys thyroid cells to slow the production of thyroid hormones.
In severe cases, the thyroid may be surgically removed, and patients will begin a Thyroid Hormone Replacement Therapy program to receive thyroid hormones.
Goiter
Goiter occurs when the thyroid grows too large. The entire thyroid may enlarge and be smooth to the touch, or the thyroid may grow nodules that you can feel through your skin. Nodules are sacs of fluid attached to the gland.
Goiter can have numerous causes, including other thyroid conditions like Hashimoto’s and Graves’ disease. It may also be caused by an iodine deficiency. Iodine is a crucial material in the production of thyroid hormones.
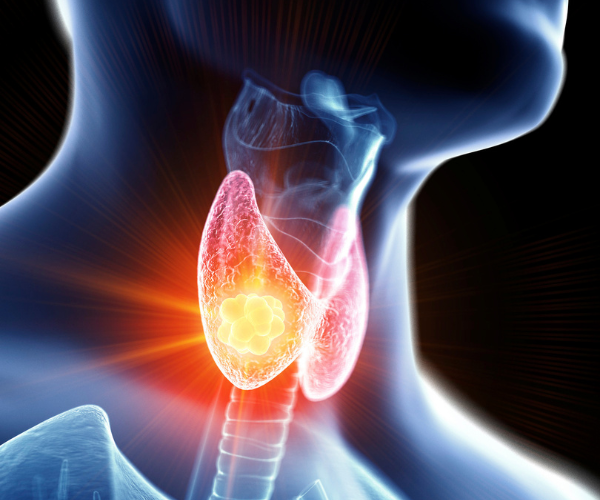
Thyroid Cancer
Cancer in the thyroid may cause thyroid disease symptoms. A malignant tumor grows on the gland, and it may be noticeable to the touch in later stages. This type of cancer is rare, but it’s more likely to occur in people aged 20 to 55.
Treatment for thyroid cancer includes surgery, radioactive iodine therapy, radiation, and chemotherapy.
If the thyroid is damaged by the cancer or treatment, patients may also require Thyroid Hormone Replacement Therapy to replenish their hormone levels.
Hypothyroidism Medication and Treatment
The most common form of thyroid treatment is Thyroid Hormone Replacement Therapy.
This treatment supplements thyroid hormones when the body doesn’t produce enough on its own. Conditions like Hashimoto’s Disease, thyroiditis, goiter, thyroid cancer, and others may require replacement of thyroid hormones.
There are different types of thyroid hormone medications, along with numerous protocols depending on what you need. There are two main forms of thyroid hormone replacement medication: desiccated and synthetic.
This medication is made of dried hormone glands, typically from pigs. It’s sometimes called thyroid extract or natural thyroid. The most common brand-name medication for desiccated thyroid hormone is Armour Thyroid. There are also compounded options.
This medication is lab-created medication that mimics the effects of thyroid hormones. Synthetic thyroid hormones are typically bioidentical, meaning they have the same chemical makeup as the thyroid hormones produced by the body.
The most popular commercial medication for synthetic thyroid hormone is Synthroid. Compounded versions include Levothyroxine (T4) and Liothyronine (T3).
Desiccated or Synthetic: Which One is Right for Me?
Studies show there is not a significant difference between the effects of desiccated thyroid hormones and synthetic. Desiccated thyroid may offer modest weight loss benefits, although this effect has not been well studied.
Synthetic thyroid hormones like Levothyroxine and Liothyronine have more clinical trials and are more commonly used. Because these medications are bioidentical, they function very similarly to natural T3 and T4.
Desiccated thyroid hormone has not been approved by the FDA due to a lack of medical studies supporting its efficacy. Levothyroxine has been approved by the FDA for the treatment of hypothyroidism.
Is one more expensive than the other?
Of the two types of medications, desiccated thyroid hormone is typically more expensive. Compounded alternatives are often more affordable than brand names for both desiccated and synthetic thyroid medication.
If you’re using insurance to cover the cost of your treatment, your insurance plan may not cover desiccated thyroid medication, since it’s not FDA-approved. If you’re interested in more in-depth thyroid treatment, your insurance company’s coverage may not be enough, either.
Defy Medical offers concierge care with no insurance-related surprises. Since we do not accept insurance, we’re able to provide leading-edge, comprehensive Thyroid Disease treatment at predictable prices.
Thyroid Hormone Replacement Therapy: Do I need T3, T4, or Both?
The thyroid creates two hormones, T3 and T4. It makes these hormones from iodine and stores and secretes them based on the body’s needs. Thyroid disease interrupts this process, leading to over- or under-production of T3 and T4.
Thyroid Hormone Replacement Therapy replenishes thyroid hormone levels by supplementing what the body doesn’t produce. But which hormones do you need?
To understand that, we’ll dive into how the body uses these hormones.
T3 and T4 in the Body
T4 is produced in large quantities by the thyroid, and it circulates in the blood until it’s needed.
T4 is converted to T3, the more potent thyroid hormone. Most T3 comes from converted T4, while a small portion of it is produced by the thyroid directly.
Because of this process, supplementing solely with T4 can be an effective treatment for hypothyroidism. However, for severe conditions or conditions in which the patient has trouble converting T4 to T3, a combination may provide better results.
Desiccated thyroid medication usually contains a mix of T3 and T4. Synthetic hormones come in the form of T3, T4, or a combination of both. Combination medication is also available in different ratios of T3 and T4.
Learn more about T3 and T4 supplementationWhich Medication is Right for You?
Ultimately, your care plan will depend on your needs, test results, symptoms, and response to treatment.
For Thyroid Hormone Replacement Therapy, it’s important to regularly follow up with a knowledgeable provider who can guide your protocol and make adjustments as necessary.
Follow-up blood testing is also recommended to make sure you’re responding positively to treatment.
Get Started
Treatments for Hyperthyroidism
Hyperthyroidism is the overproduction of thyroid hormones, and it’s treated differently than hypothyroidism.
When the thyroid produces too much T3 and T4, therapy is geared toward slowing that production. There are several ways to do this.
Hyperthyroid Medications
To treat thyroid hormone overproduction, there are medications called antithyroids or thionamides. These make it harder for the thyroid to produce thyroid hormones, especially T4.
There are two main types of thionamides:
This medication comes in pill form and is typically taken once per day. For most patients, it lowers the amount of T4 levels to normal ranges in six weeks. It can be used as a monotherapy for hyperthyroidism, or as a preparatory therapy given to patients prior to radioactive iodine treatment or thyroid surgery.
This medicine comes in tablet form and is typically taken multiple times a day. Propylthiouracil begins changing thyroid production within the first few days, but usually reaches peak effectiveness at around 8-12 weeks. Propylthiouracil has more side effects than Methimazole, so it’s often prescribed if the patient hasn’t had success with Methimazole.
Radioactive Iodine
Radioactive iodine functions by destroying some or all of the thyroid, thus slowing the production of thyroid hormones.
The thyroid absorbs the majority of circulating iodine, so radioactive iodine is specifically targeted to this gland. Once your thyroid cells take in the iodine, they begin to die. This may occur in some or all of the cells, depending on the treatment and severity of your hyperthyroidism.
Radioactive iodine is available as a pill or liquid form. Most patients only need one dose of the medication. You may feel a reduction of symptoms within the first month, with full relief starting up to six months after your dose.
Recent studies have observed a potential connection between radioactive iodine and increased risk of cancer and infertility. Concerned patients may wish to pursue other treatments for hyperthyroidism.
Thyroid Removal Surgery
This surgery is called a thyroidectomy and it removes part or all of the thyroid gland.
A thyroidectomy is the most serious treatment for hyperthyroidism and is typically considered after other treatments have failed. It’s also performed on patients with thyroid cancer, goiter, thyrotoxicosis, and other serious thyroid conditions.
There are three thyroidectomy levels:
- Partial thyroidectomy where only part of the thyroid is removed.
- Near-total thyroidectomy, where most (but not all) of the thyroid is removed.
- Complete thyroidectomy, where all of the thyroid is removed.
Thyroidectomies are considered major surgery and will be performed at a hospital or outpatient surgical setting. Doctors may use less invasive techniques like special instruments to minimize the surgical incision. Some thyroidectomies require full open surgery depending on the severity of the condition.
Recovery times vary depending on the type of surgery.
Patients who undergo a thyroidectomy typically need Thyroid Hormone Replacement Therapy afterwards to provide their body with necessary thyroid hormones.
Thyroid Disease Treatment at Defy Medical
Defy Medical offers individualized treatment for hypothyroidism and hyperthyroidism.
Through Defy Medical, you can access comprehensive blood testing to diagnose a thyroid issue, in-depth consultations to help you understand your treatment, and medication to bring your thyroid hormones into balance (as appropriate).
Ready to learn more?
Get Started